I often watch blooper shows such as MTV’s Ridiculousness and wonder in bewilderment what the entertainment value is in watching a skateboarder cracking his head against a sidewalk or two drunks knocking each other out with devastating punches. Or, for that matter, the recent and completely absurd urban “knockout” trend of punks arbitrarily walking up to an unsuspecting pedestrian and punching them in the face with the sole goal of rendering them unconscious.
The fact of the matter is that there is nothing amusing or entertaining about a head injury, especially one that results in what is defined as traumatic brain injury (TBI). This phenomenon has been borne out in this recent generation of combat vets returning from improvised explosive device (IED) attacks in Iraq and Afghanistan. A study conducted by researchers with the Veterans Administration Puget Sound Health Care System and the University of Washington estimates that between 10 and 20 percent of the 2.6 million who served in the recent combat zones returned with post-concussive symptoms.
You don’t need to be in combat or on a playing field to be exposed to this significant threat. Each year, there are approximately 1.7 million new cases of TBI diagnosed, and 50,000 of those result in the patient’s death. The causes can range from accidents at home or in motor vehicles to participation in many sports to acts of violence and severe weather events.
What makes these injuries especially confounding, both for the victim and healthcare workers, is that the seriousness of these injuries doesn’t always appear immediately or even seem to be severe. If you’re in a survival situation, you’ll probably be more likely to encounter this type of injury than you are today.
This is a list of some of the fundamental warning signs that a TBI has occurred:
- No loss or temporary or prolonged loss of consciousness. Anytime there is a loss of consciousness, there is no need to guess whether a TBI has occurred … it has.
- Orientation to person, place or time. Does the victim know who they are, where they are what day it is?
- Headache
- Amnesia
- Confusion
- Nausea
- Dizziness
- Ringing in the ears (tinnitus)
- Inability to concentrate
- Eyes sensitive to light
- Irritability
- Loss of appetite
- Lethargy
Unsteadiness. One battery of tests athletic trainers give on the sidelines resembles those used by police to determine whether a driver is intoxicated. Refer to the accompanying images to learn how to perform these simple tests.
These symptoms typically last a short time, but if there is ever any doubt, seek medical attention.
The TBI becomes critical and potentially life-threatening when the following occur:
- Worsening headache
- Persistent/projectile vomiting
- Unequal pupils. This is where one is extremely dilated and the other either remains the same or is more constricted.
- Seizures
- Unconsciousness
- Labored breathing
For instance, consider the high school football coach who works with an athlete who took a hard shot to the head but doesn’t get knocked out. He shrugs it off as a short-term inconvenience of his player “getting his bell rung.” He lets the player shake it off and then allows him to return to the game. Or, when a bicyclist falls in the street, hits their head on the pavement and suffers blurred or double vision. Despite the presence of an increasing headache, they self-treat with ibuprofen and fail to seek medical attention.
After a 22-year career as an athletic trainer who worked with athletes from pee-wees to Olympians, all I can say about the above protocols is, “Wrong!” In fact, 25 years ago, I was considered a heretic when I wrote an article for a coaching magazine raising concern about the repeated effects on the brain from heading the ball in soccer.
With a sense of redemption, I noted that many youth soccer leagues in the United States have now banned this move after research has recently shown that there are long-term effects of cognitive brain function affecting memory and simple problem-solving among veteran soccer players.
Traumatic vs. Chronic Injuries
For the sake of this article, it is important to distinguish between traumatic and chronic injuries.
“Traumatic” refers to the initial event that results in some kind of neurological disruption. It could be from a direct blow to the head or a whiplash motion, causing what is referred to as a “contrecoup injury.” We typically call this a concussion. Not all concussions result in unconsciousness.
I have lost count of arguments I had with coaches who said their player was OK, simply because he wasn’t knocked out. Regardless, these would be considered TBIs.
The chronic cerebral phenomenon is referred to as chronic traumatic encephalopathy. This is from repeated blows to the head resulting in a degenerative disorder of neural function. This was succinctly portrayed in Will Smith’s movie, Concussion, which highlighted the effect of this condition on NFL players. The Department of Veterans Affairs at Boston University identified 87 deceased former players with this malady.
The brain is comfortably encased in the human helmet called the cranium—your skull. But, while the skull provides some protection, the brain is essentially suspended in cerebrospinal fluid and connecting veins and arteries. I typically compare this to a bowl of Jello. You may be able to hit the side and it will provide some degree of protection but hit it hard enough or shake the bowl, and you can see how the Jello is affected. The brain acts in a similar fashion, and injuries could result in temporary or permanent disability or even death.
Because TBI is often difficult to assess in victims—let alone when it occurs to yourself—seeking medical attention is always recommended.
- DO NOT take ibuprofen, which could actually increase any bleeding that occurs. Some doctors recommend Tylenol, but take note that it could mask the severity of the injury.
- If you are going to lay down, be sure the head is above the level of the body—not with the feet elevated, which could increase intracranial pressure.
- An ice pack to the back of the neck might relieve some neck tension that could increase the headache.
The key to TBI first aid is to avoid further contact to the head. This is the reason that great caution is now being exercised in the NFL with the concussion protocol it now follows.
Delayed Effect of Serious Brain Trauma
What is scary about TBI is that death might occur without an indication that a serious brain injury has been sustained. There have been numerous incidents when an athlete sustained a seemingly minor head injury early in the week but died on the field later in the week after sustaining a subsequent, even relatively minor blow.
In 2013, 16-year-old football player Dodi Soza of Downey, California, suffered a concussion in practice two days before a game during which he was struck in the head, collapsed and died. Five years earlier, Ryne Dougherty, 16, of Montclair, New Jersey, died two days after sustaining a hit to the head in a junior varsity football game.
The list is long and horrifying, but steps can be taken to help mitigate the incidence and severity of head trauma through understanding the mechanism of injuries, knowing the warning signs and what to do when they occur.
Causes of TBI—the Mechanism of Injury
Direct hit to the head. This can result from a punch in a bar brawl, falling down a flight of stairs or the side of a hill, being hit by debris in a storm, suffering an impact in a motor vehicle accident or hitting the head while playing a sport or any other everyday activity.
Indirect force to the brain. It is often tricky for a victim to connect the dots, because they will manifest the signs and symptoms of a TBI, even though they didn’t hit their head.
Using the Jello analogy, the brain isn’t as well protected as most people believe. So anytime a force is transmitted through the body to the brain, a TBI can occur. For example, a whiplash action, during which the head is violently whipped forward/backward, side to side or rotationally can result in a TBI. Falling hard on the butt can generate enough force through the spine to affect the brain. A punch in the jaw, while not thought of as connected to the brain, can also cause the brain to slosh inside the skull. Some veterans who were exposed to IEDs were victims of a blast trauma, which can cause traumatic brain injuries without a direct impact to the head.
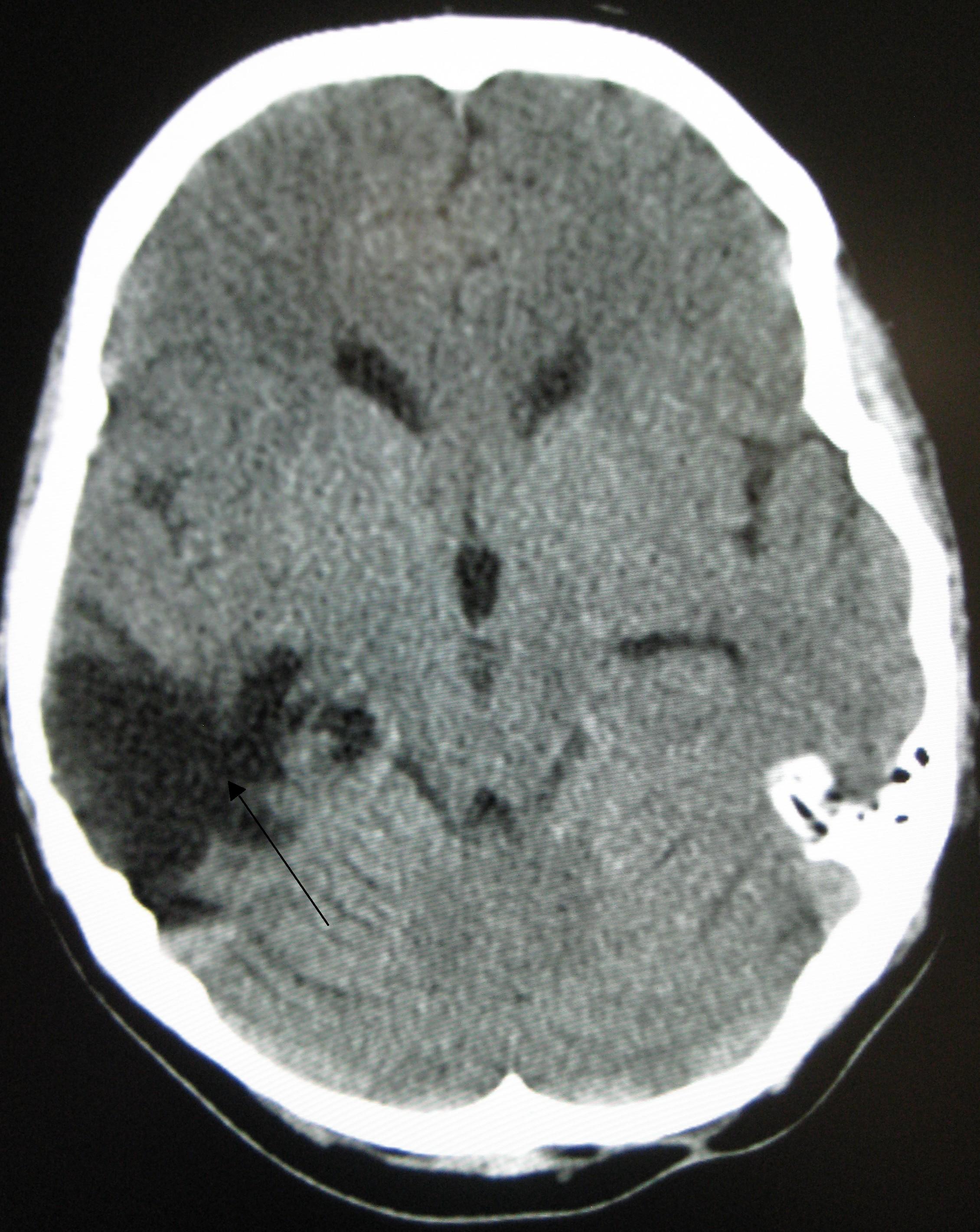
What actually happens to the brain in these scenarios is still a source of contention among scientists. A concussion is essentially defined as a “temporary disruption in brain function.” Unconsciousness does not always ensue, but in more severe cases, it can. The individual runs into trouble when bleeding occurs, either between the brain and the skull (“epidural”) or when the blood pools between brain layers (“subdural”). The more bleeding there is, the more pressure is put on the brain and the greater risk of death.
Returning to contact too soon, while still experiencing headaches and other symptoms, can be deadly. This is no time for self-negotiating to gamble with your life. The risk of “second impact syndrome” is serious. This might occur when the brain sustains another injury before it has fully recovered from the initial blow. This can even happen weeks after the first concussion was suffered.
At no time should there be a return to activity if any of the above symptoms exist. Once they disappear, the following protocol—similar to the one employed by the NFL—should be followed:
- Rest and recovery: This will allow for the removal of symptoms. Avoid watching TV, video games, social media or doing computer work.
- Light aerobic exercise: Try 10 to 20 minutes of light stationary cycling or walking, monitoring any resurgence in symptoms. Stop if they re-appear. More rest will be required.
- Continued aerobic exercise and introduction of strength training: Increase the level of aerobic activity and incorporate light weight-lifting.
- Sport-specific activities: The cognitive load of playing the sport will be added, and the individual will participate in non-contact activities for the typical duration of a full practice.
Full activity/clearance: A player returns to full participation in practice, including contact without restriction.
Prevention Is Key
The first step in preventing TBIs is effective head protection. It is amazing that there are only 19 states that require all motorcycle riders to wear helmets where the rest either don’t have laws or only require helmet use by riders under 17 or 20 years old.
There is a growing trend in many sports toward the use of head protection; this includes goalkeepers in soccer and pitchers and base coaches in baseball/softball. The appreciation for bicycle helmets has increased exponentially in recent years.
But with all this appreciation, a helmet does little good if it doesn’t fit properly. No longer is the sight of a pee wee football player running downfield with his helmet wobbling over his eyes considered cute. Helmets should fit snuggly but not so tight as to cause a headache. The front rim of the helmet should be two finger widths above the eyebrows. The chin strap should always be fastened. When everything is in place, carefully shake the helmet forward and backward and then try to rotate it. There should be minimal to no movement.
TBIs occur more frequently than most people realize. Their severity can range from minor and temporary to life-threatening. Appreciating the need for protection, along with early identification, treatment and knowing when to safely return to activity, can make a huge difference in your well-being.
– Joseph J. Kolb, M.A.